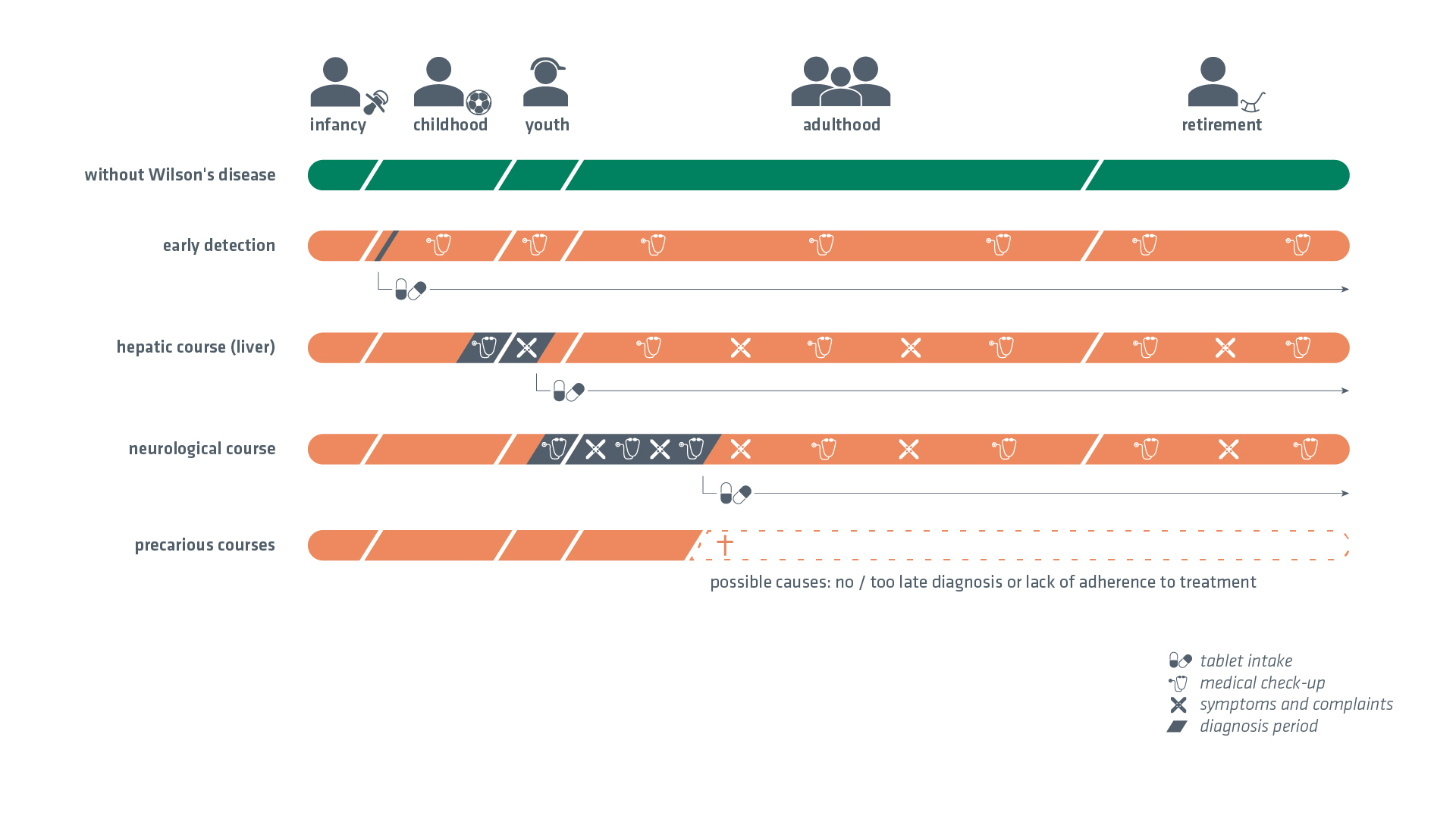
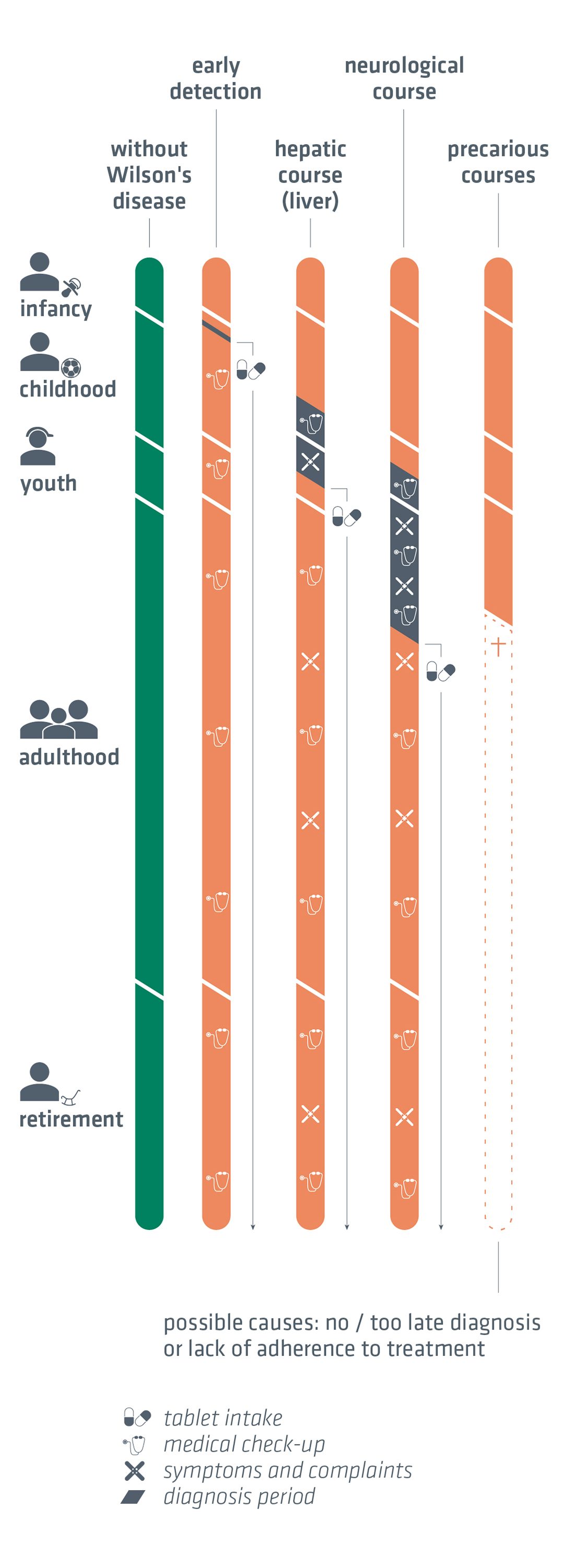
The type and severity of the symptoms of Wilson's disease can be very different. Therefore, the course of life with this disease is very individual. Nevertheless, two typical symptomatic courses can be distinguished: The hepatic (affecting the liver) and the neurological or neuropsychiatric course.
The extent of the symptoms increases with the age at diagnosis. In childhood and adolescence, damage of the liver usually takes centre stage. In (early) adulthood, neurological symptoms also occur. Due to the rarity of the disease, many patients have a long and sometimes arduous journey from the first symptoms to diagnosis.
In the non-symptomatic form, the disease is diagnosed before the onset of the actual symptoms. This occurs, for example, when the other family members are tested for the disease because Wilson's disease has already been diagnosed within a family.
Treatment of this disease is both possible and necessary. Regardless of how severe or mild the symptoms of Wilson's disease are, it is crucial that patients take their medication reliably and, if possible, at the same time as their meals. This is one of the most important pillars of successful therapy. Neurological patients have a chance of improving their symptoms through drug therapy. However, there are also forms of the disease in which patients have to cope with the neurological symptoms for the rest of their lives despite treatment.
If the diagnosis can be made early and the disease is treated consistently throughout life, the prospects for a ‘normal’ life with Wilson's disease are very favourable. Patients are predicted to have an average life expectancy with treatment.
The therapy must be carried out for life!


Therapy
Drug treatment (primary therapy)
Small amounts of copper are present in almost all foods. Wilson's disease patients are therefore treated by taking pills that prevent the copper ingested with food from accumulating in the liver and from there in the brain.
In Germany, the active agents D-penicillamine, trientine and zinc are used for primary drug therapy. In this context, D-penicillamine and trientine are so-called copper chelating agents. These substances are able to bind copper ions and thus eliminate them as potentially dangerous substances for the body. The copper bound in this way is excreted in the urine via the kidneys. The other strategy is to administer zinc-containing substances to those affected. The administration of zinc inhibits the absorption of copper in the intestine and thus also slows down its accumulation in the body. Copper from food is excreted in the faeces during zinc therapy.
For acutely ill people with Wilson's disease (typically newly diagnosed patients with symptoms), D-penicillamine and trientine are primarily recommended at the start of treatment in order to decopperise the body. Zinc is also used for maintenance medication after the acute phase of the disease has been overcome or for therapy in the case of incidental findings (e.g. sibling examination).
All of these medications are usually taken in several single doses throughout the day on an empty stomach, i.e. 1-2 hours before or 1-2 hours after meals.
Drug treatment during pregnancy
ATTENTION: Treatment must not be interrupted during pregnancy. Discontinuation of therapy is life-threatening!
The German Wilson’s disease association offers the flyer ‘Pregnancy and breastfeeding with Wilson’s disease‘ free of charge for prospective mothers.
Nutrition
A healthy and varied diet is recommended. A strict low-copper diet is not absolutely necessary if the primary therapy is stable. If, despite good drug therapy, the copper metabolism is insufficiently controlled, an increased low-copper diet can provide support. This is primarily used for newly diagnosed patients, who usually have a lot of stored copper in their bodies. Copper-rich foods such as seafood, pluck, nuts, sultanas, almonds and cocoa-containing foods such as chocolate should be avoided. Designer food (energy bars, food supplements, multivitamin tablets) can also contain a lot of copper and should only be consumed after carefully reading the ingredients.
Members can find a list of foods in our member area.
ATTENTION:
Copper CANNOT be removed from the body by diet. A low-copper diet can NEVER be an effective therapy on its own. Drug therapy is the only way to remove copper from the body!
ATTENTION:
Like any person with a damaged liver, it is advisable for Wilson's disease patients to avoid alcohol completely.
Drinking water
Drinking water from the public supply networks is tested and safe. Possible tap water residues can be largely avoided by running tap water in advance. Drinking water from private wells should be checked.
Vitamins and trace elements
Vitamin B6 supplementation is recommended for patients undergoing D-penicillamine therapy (20 mg 3 times a week). Otherwise there are no general recommendations, except in cases of proven deficiency of trace elements or vitamins.
Further therapeutic approaches
Transplantation: As Wilson's disease is primarily a liver disease, liver transplantation is also an option for treating the acute form of the disease, particularly in cases of fulminant liver failure. The number of transplants carried out in Germany is very low.
Gene therapy: Several companies are conducting clinical trials on gene therapies they have developed (as of 2024).
Physiotherapy / occupational therapy / speech therapy / psychological support therapy
These therapies are very useful for proven functional disorders / psychological stress.
Alternative medicine
This can be dangerous. Chinese or Ayurvedic teas, for example, can contain large amounts of copper. We recommend that you consult a specialised Wilson’s disease centre.
Travelling with medication
If you wish to take large quantities of your medication with you in your hand luggage when travelling abroad for a longer period of time, you may encounter problems at customs or at the security check of your hand luggage. In order to be as prepared as possible for such a situation, it is advisable to ask your doctor for a certificate confirming the need to take your medication (in English if necessary), which you can take with you when travelling.


Follow-up check
For all people with Wilson's disease, regular medical check-ups in an internal medicine and/or neurology outpatient clinic are of great importance. This serves to check the effectiveness of the therapy administered and can also provide patients with valuable feedback on how they are dealing with their therapy. Those affected usually have to travel a long way to get there, as there are only a few centres specialised in Wilson's disease in Germany.
Who is the contact person?
A specialised centre should be contacted about 1 to 2 times a year. Whether primary neurological or internal/hepatological care is better depends on the main symptoms.
In the SE-Atlas for ‘Wilson's disease’, most of the listed facilities for Wilson's disease can be found well-structured on a map here.
All known to us specialists and addresses that can be contacted for Wilson's disease can be found under Specialists.
What should the follow-up check include?
- Patient interview: Questions and complaints may need to be noted beforehand
- Patient examination (side effects of the therapy?)
- Laboratory tests:
- Blood count
- Liver values
- Quick value
- Coeruloplasmin in serum
- Copper in serum
- 24-hour urine collection for copper (also for zinc under zinc therapy)
- In a specialised centre:
- Ultrasound liver and spleen
- Specialised neurological examinations if necessary
- Follow-up check Kayser-Fleischer ring by ophthalmologist (if present at the time of diagnosis)